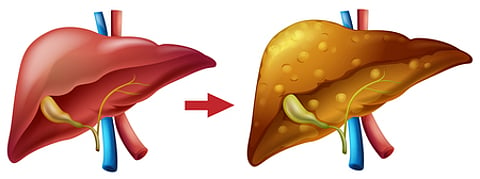
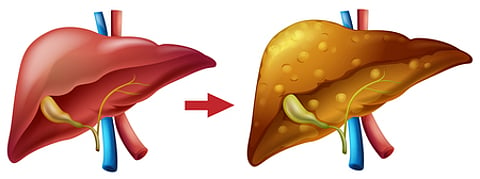
NEW DELHI: With Asian Indians facing a rising 'dual epidemic' of Type 2 Diabetes (T2D) and Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), top Indian medical experts have released new consensus guidelines tailored specifically for this high-risk population.
Published in the journal Diabetes and Metabolic Syndrome: Clinical Research and Reviews by Elsevier, the guidelines offer evidence-based recommendations for the diagnosis and management of MASLD in Asian Indians with coexisting T2D—two conditions that significantly aggravate each other.
“These guidelines are necessary because Asian Indians show unique metabolic characteristics with higher liver fat deposition than other ethnic groups. India faces a ‘dual epidemic’ of T2D and MASLD, with each condition worsening the other,” said Dr Anoop Misra, Chairman of Fortis CDOC Center of Excellence for Diabetes, Metabolic Diseases and Endocrinology, New Delhi, and lead author of the guidelines.
MASLD, previously known as non-alcoholic fatty liver disease (NAFLD), has become the most common cause of chronic liver disease globally. In India, its prevalence ranges from 27.7% to 88.6% across different population subgroups. Among high-risk Asian Indians—those with obesity, diabetes and other metabolic conditions—the prevalence reaches 52.8%, compared to 28.1% in average-risk individuals, according to a systematic review and meta-analysis cited in the document.
“While guidelines exist for MASLD globally, none specifically address management in individuals with T2D,” said Dr Misra, recipient of India’s highest medical honour, the Dr B.C. Roy Award in 2006, and the Padma Shri in 2007.
MASLD is not only the leading cause of liver-related morbidity and mortality but also an independent risk factor for cardiovascular disease—the primary cause of death in this demographic.
The new guidelines, developed in collaboration with senior doctors from institutions such as AIIMS, Sir Ganga Ram Hospital and Medanta, recommend routine MASLD screening for all T2D patients, especially those with high-risk features like metabolic syndrome and obesity.
“Clinical evaluation should include BMI, waist circumference and waist-to-height ratio, with non-invasive tests like FIB-4 and liver stiffness measurement to assess fibrosis,” said Dr Misra, who also heads the National Diabetes Obesity and Cholesterol Foundation (N-DOC).
Weight loss is identified as a critical intervention, improving outcomes for both MASLD and liver fibrosis. The guidelines recommend lifestyle modifications, including a diet comprising 50–60% complex carbohydrates, 20–30% fats (primarily unsaturated), and 15–20% proteins. They advise limiting saturated/trans fats, refined carbohydrates and added sugars.
A plant-based diet is encouraged, incorporating legumes, nuts and seeds, which are rich in dietary fibre and essential nutrients that support liver health and reduce inflammation.
For non-vegetarians, the guidelines recommend fish and seafood—particularly fatty varieties like salmon and mackerel—due to their omega-3 polyunsaturated fatty acids (PUFAs). In contrast, red and processed meats should be minimised or avoided due to their link to MASLD progression.
Other key recommendations include engaging in 150–300 minutes of moderate or 75–150 minutes of vigorous physical activity per week, and complete avoidance of alcohol.
The experts—Dr Ashish Kumar (Professor and Senior Consultant, Gastroenterology and Hepatology, Sir Ganga Ram Hospital), Dr Mohammad Shafi Kuchay (Senior Consultant, Endocrinology and Diabetes, Medanta), Dr Narendra Singh Choudhary (Associate Director, Hepatology, Medanta), and Dr Naval K. Vikram (Professor, Internal Medicine, AIIMS Delhi)—also pointed to the harmful impact of certain fats prevalent in Indian cooking.
They warned that high consumption of saturated fatty acids (SFA) and trans fatty acids (TFA), especially from ultra-processed foods and repeatedly heated edible oils, contributes to hepatic fat accumulation, insulin resistance and inflammation.
“It is crucial to limit oils high in saturated fats (ghee, coconut oil, palm oil, butter, cream, animal fat) and omega-6 PUFAs, as excessive intake has been linked to inflammation and liver fat accumulation,” the experts said.
Regular coffee consumption—more than three cups per day, particularly caffeinated and brewed varieties—was associated with improved liver enzymes, reduced liver fat and decreased inflammation.
“The guidelines provide clinicians with a practical framework for managing MASLD in people with T2D, accounting for the unique metabolic characteristics of Asian Indians. It offers specific, evidence-based recommendations for screening, assessment frequency, and interventions, with clear algorithms facilitating clinical decision-making,” said Dr Misra.
He added that the guidelines also outline when to refer patients to specialists and offer a comprehensive roadmap to target both glycaemic control and liver health.