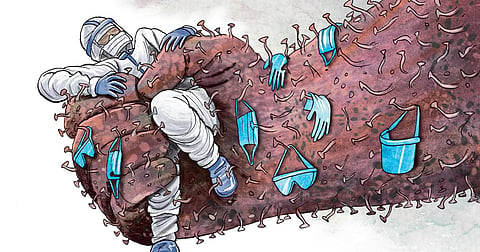
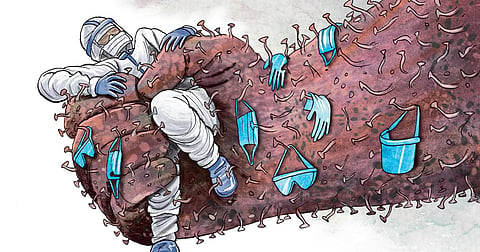
The current global crisis due to the coronavirus has brought the healthcare community and its work-related problems into focus. While the prime minister has rightly lauded their contribution, the occupational health problems of healthcare workers have always been neglected not only by authorities but also by doctors themselves. They are the most vulnerable group on whose health the Covid-19 control strategy rests.
In current times the problem has become serious. According to FNOMCeO, Italy’s main doctors’ association, at least 100 doctors in that country have already died of Covid (as on April 9). In Spain, more than 10% of diagnosed Covid cases are doctors or nurses. The National Health Commission of China reported that up until February 24, 2,055 healthcare workers had been confirmed infected with Covid, with 22 deaths in that nation. According to reports, more than a dozen doctors have contracted the disease in five Indian states. Recent reports indicate that 48 healthcare workers including four doctors of two prominent hospitals in Mumbai have tested positive.
In a recent study of 4,357 healthcare workers in Wuhan, the main concerns reported by health workers were: infection of colleagues (72.5%), infection of family members (63.9%), protective measures (52.3%) and medical violence (48.5%). And 39.1% of healthcare workers had psychological distress.
The data on the morbidity and mortality experienced by healthcare workers in India is lacking as reliable statistics are not available. Even large teaching hospitals and medical colleges do not have an occupational health department. Hospitals are also not required to collect and report data on hospital-acquired infections in its staff. There is no specific legal requirement for comprehensive occupational health services in hospitals in India. Even the medical community and unions have seldom made demands for protecting their health and safety except for protection from violence in recent years. Workplace violence has emerged as an important threat in healthcare over the last few years. Though agitations by doctors forced the government to enact a nationwide law, it has failed to significantly change the situation on the ground so far.
Occupational health problems can be prevented with the help of universal precautions. The risk of infection increases due to lack of sufficient PPE (Personal Protective Equipment) and inadequate training further amplifies the risk of infection in healthcare workers. Proper PPE plays the most important role. It has been reported from Wuhan that the Covid protective gear was so cumbersome and expensive that healthcare workers were forced to use adult diapers during their shift so that they do not have to take off the PPE.
Training and education of healthcare workers and extensive medical surveillance are very crucial. Long-time exposure to large numbers of infected patients directly increases the risk of infection. Also, pressure of treatment, work intensity and lack of rest indirectly increase the probability of infection. It is essential to identify, monitor and control exposures of healthcare workers and also offer them preventive immunisations on priority as and when available, e.g. for Hepatitis B.
Stress management plays a major role considering the enormous pressure to which healthcare workers are exposed. Videos coming out of Chinese and Italian hospitals are graphically showing how much more stressed health workers can be due to the overwhelming pandemic. Dealing with life and death, and round-the-clock work are the hallmark of healthcare jobs and both are stress generators. The development and implementation of mental health assessment, support, treatment and services are crucial in the health response to the coronavirus outbreak.
Our healthcare set-ups in the state sector are perpetually saddled with manpower shortage and perceived lack of support from the state. The new trend of outsourcing/on-contract workers in various industries has been extended to healthcare not only in the private sector but also in the government. The savings come at a tremendous cost in terms of quality of manpower and consequently the quality of care. There is a strong need to improve the monetary compensation and working conditions of staff in health facilities.
Besides respectable and attractive salaries, proper on-campus accommodation, timely promotions and non-monetary recognition are essential, and changes in the system are required. Every large hospital should have a dedicated and qualified occupational health professional. The occupational health of healthcare workers is not yet a priority for stakeholders. This has resulted in increased risk and decreasing attraction in medicine as a career.
Given our huge population and shortage of healthcare workers, the situation needs to be addressed by improving working conditions, using innovative human resource policies and structural reforms. Health departments should regularly report the number of infected and dead healthcare workers along with the total Covid-19 infections and deaths. Each incident of a healthcare worker being infected should be investigated and the flaws that led to it should be immediately fixed. This is essential for a healthy India.
Dr Shyam Pingle
Senior Occupational Health Advisor, Indian Institute of Public Health, Gandhinagar. Views are personal
Email: shyampingle@iiphg.org