Gastroesophageal reflux disease: When food spills out of stomach
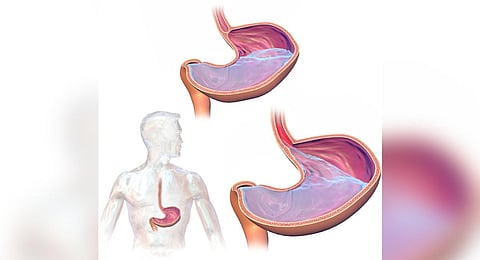
BHUBANESWAR: If you experience a burning sensation in the chest, usually after having food, or have upper abdominal pain and trouble in swallowing (dysphagia) or feel a lump in the throat, do not ignore it, as you may have or end up with gastroesophageal reflux disease (GERD), commonly known as acid reflux. Usually, the food we swallow reaches the stomach through the oesophagus and the muscle fibres at the lower oesophagus prevent the food from moving back up. But when the ring of muscle does not close all the way, stomach contents can spill back into the oesophagus. This condition is called reflux or gastroesophageal reflux, and frequent acid reflux causes GERD.
GERD occurs when stomach contents repeatedly flow back into the oesophagus (food pipe). This backwash irritates the lining of the esophagus leading to heartburn and pain. Although heartburn is a symptom of acid reflux, it has nothing to do with the heart.
As per studies, the prevalence of GERD ranges from 7.6% to 30% in the Indian population and around 22.2% in southern states. It is more common in the elderly, obese people, alcoholics and smokers, and also during pregnancy. People residing in urban areas are more vulnerable to the disease than those in rural areas.
GERD is most familiar in western countries, affecting around 20% of the population and about 60% among them are women. The dietary factors associated with the disease include intake of spices and meat. Less than 10% of GERD patients in India have erosive esophagitis.
Dr Sushant Sethi, head of Institute of Gastroenterology at Apollo Hospital, Bhubaneswar, said GERD is one of the most common gastrointestinal disorders these days due to changing food habits and lifestyle. “Acid reflux cases are not uncommon these days, but some people suffer from burning discomfort, bloating and belching almost every time they eat. It can lead to scarring of the tissue in the oesophagus and gets worse if not diagnosed and treated early,” he said.
Causes and symptoms
GERD may develop if the lower esophageal sphincter becomes weak or relaxes when it should not. Factors that can aggravate acid reflux include smoking, eating heavy meals or eating late at night, eating certain foods (triggers) such as fatty/non-vegetarian or fried foods, drinking beverages such as alcohol.
Some medicines can also cause GERD or make its symptoms worse. Unregulated use of benzodiazepines, sedatives that make people calmer or sleepy, calcium channel blockers - which are used to treat high blood pressure, certain asthma medicines, non-steroidal anti-inflammatory drugs, painkillers, sedatives and antidepressants can lead to gastroesophageal reflux disease.
Bengaluru-based senior gastrointestinal surgeon Dr Muralidhar S Kathalagiri said poor lifestyle decisions, stress, insufficient sleep, weight gain and improper eating practices are some of the causes of rising prevalence of GERD in metropolitan settings. “Younger people are now suffering from GERD, most likely because of elevated stress levels. This emphasizes on a healthy lifestyle and raising awareness about GERD,” he said.
Symptoms
The disease can manifest in a wide range of symptoms which can be divided into typical, atypical and extraesophageal symptoms. Typical symptoms include heartburn and acid regurgitation. Among atypical symptoms, epigastric pain, dyspepsia, nausea, bloating, excessive burping and belching are common.
Those who have night time acid reflux, they might also experience ongoing cough, inflammation of the vocal cords (laryngitis) and new or worsening of asthma. Over time, chronic inflammation can cause inflammation of the tissue in the esophagus (esophagitis). Frequent flow of acid can also cause changes in the tissue lining of the lower esophagus and lead to risk of esophageal cancer.
“Overstress or a bad lifestyle will worsen these symptoms. Individuals in their late 30s and 40s are more likely to experience the disease,” Dr Kathalagiri stressed.
Diagnosis
GERD is broadly categorised into four types – mild, moderate, severe and pre-cancer or cancer. In mild GERD, acid reflux occurs once or twice a month while in moderate, symptoms are frequent enough to require medication, which is typically taken daily. If the symptoms persist despite medication, it can become severe and later cancerous.
The diagnosis is typically made by a combination of clinical symptoms, response to acid suppression, as well as objective testing with upper endoscopy and esophageal pH monitoring. Patients with symptoms of GERD, such as heartburn and regurgitation, can be diagnosed and treated empirically with proton pump inhibitors (PPIs). Diagnostic procedures include x-ray of the upper digestive system, upper endoscopy, reflux testing (wireless pH/pH impedance), esophageal manometry, barium esophagram and transnasal esophagoscopy.
“The most common diagnostic procedure for GERD is endoscopy, which can reveal changes in the esophageal mucosa. About 30-40% of GERD patients show these changes. However, some patients may have normal-looking oesophagus on endoscopy but still experience symptoms, which is called NERD. It accounts for the majority of GERD cases (60-70%). To diagnose NERD, 24-hour pH monitoring is often used,” said Dr Bhageerath Raj D, consultant gastroenterologist, hepatologist and therapeutic endoscopist at Renova NIGL Hospitals, Hyderabad.
Treatment and management
GERD is a chronic disease that typically requires long term management in the form of lifestyle modification, medical therapy and surgical therapy for a subset of patients. Options include antacids that neutralise stomach acid, medications to reduce acid production and medications that block acid production and heal the esophagus. The mainstay of treatment is acid suppression.
Dr S Arulprakash, senior consultant and clinical lead gastroenterology at MGM Healthcare Hospital, Chennai, said advanced diagnostic procedures like 24-hour pH monitoring and esophageal manometry allow physicians to accurately diagnose and plan treatment for patients. “Mild cases can often be managed with lifestyle changes and antacids. For severe cases, PPIs or surgery may be recommended. Personalised treatment plans are crucial, as GERD can vary widely in severity among individuals. Patients, who do not respond to medicines, can benefit from endoscopy or surgical treatment,” added Arulprakash.
As GERD can be considered as a potential co-factor in patients with asthma, chronic cough or laryngitis, physicians often go for careful evaluation for non-GERD causes in these patients. “Surgical treatment may be required in cases of persistent or uncontrolled GERD. Patients are recommended for fundoplication, in which surgeons wrap the top of the stomach around the lower esophageal sphincter to tighten the muscle and prevent reflux. It also helps tighten the lower esophageal sphincter. Besides, linx device (a ring of tiny magnetic beads) can be surgically implanted at the junction of stomach and esophagus to keep it closed, but weak enough to allow food to pass,” said Dr Ayaskanta Singh, head of gastroenterology and liver sciences, SUM Ultimate Medicare.
(With inputs from Namrata Sindwani from Bengaluru, Sinduja Jane from Chennai and Renuka Kalpana from Hyderabad)